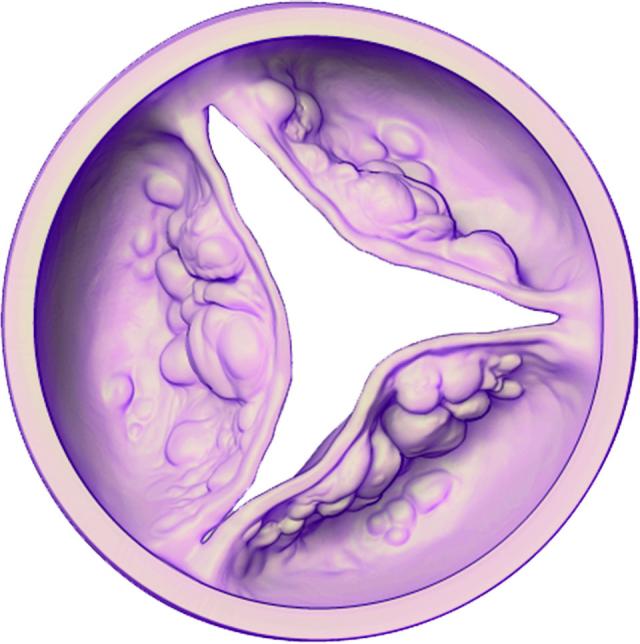
Those suffering from a potentially life-threatening disease aortic stenosis will have a better chance of accessing minimally invasive treatment.
Non surgical treatment transcatheter aortic valve implantation, or TAVI, was included on Medicare form 1 July – meaning patients experiencing the narrowing of the heart valve resulting in their heart working harder to pump blood around their body, an impact of the condition, will now have the chance to recover with reduced procedure time and a shorter stint in hospital.
Patients can also expect lower risk of complications, improved quality of life and extended life expectancy, according to cardiologists.
Phil Holmes, 72, was living in Olinda when he made the decision to undergo a TAVI on 20 September 2019 at the Alfred Hospital.
“I’d been going to gym five days a week for about seven years before I had the procedure. I was very fit and very active, [doing] two crossfit classes on a Tuesday and Thursday,” Mr Holmes said.
“A group at the gym decided to do the push up challenge – [in 2019], it was 3128 push ups in 21 days – we decided we’d do 4000 in 28 days…”
“In the third week, I really really struggled. By the time Wednesday came, I was just done… I was getting quite breathless. I didn’t know what it was but I knew something wasn’t right.”
It was then Mr Holmes sought the advice of a cardiologist, who confirmed the father of three and grandfather of five’s aortic valve was “not great” and warned he could potentially suffer a fatal heart attack at any time.
“I was really shocked because I’m only a very social drinker, non-smoker and very fit,” Mr Holmes said.
“I had the two options of either having open heart surgery, which was not appealing to me… but I also had no idea what a TAVI was… I considered the risks and decided to go ahead and have the TAVI procedure.”
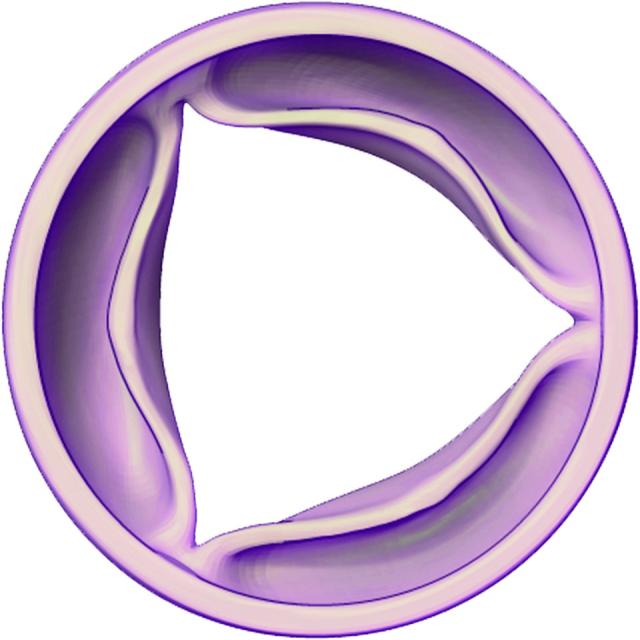
Performed by a specially trained interventional cardiologist or cardiothoracic surgeon as part of a heart team, a TAVI involves a small incision, usually in the groin, where a catheter is inserted into the femoral artery.
The artificial heart valve is then guided up to the heart and expanded into place.
“I had mine on the Friday afternoon [and] I was up eating and doing normal things on Friday night. I was walking around the hospital on Saturday, down the cafe with my wife and came home on Monday,“ the businessman said.
“On Monday afternoon, I was sitting on the couch but I was doing emails for work – I was pretty much back to work on the Tuesday, feeling fantastic. No side effects,” he said.
If not identified or treated effectively, more than half of those living with severe symptomatic aortic stenosis may die within two years, according to the report, Timing of aortic valve surgery, published in BMJ journals.
But Dr Heath Adams, interventional and structural cardiologist at the Hobart Heart Centre and Royal Hobart Hospital said the progession rate of the disease was fortunately very slow.
“It’s also important to emphasise that symptoms can’t be blamed on old age alone,“ Dr Adams said.
“If patients notice they’re more short of breath than usual, they’re more fatigued than usual, if they experience chest pain or blackouts, they need to be assessed by their GP and they need to have their heart listened to with a stethoscope.“
“If there’s a suspicion, they can have something called an echocardiogram, which [involves] rubbing gel on the chest wall and taking pictures with an ultrasound – and that will give a diagnosis if that’s what the patient is suffering from.“
Dr Adams said up until 2017, the TAVI was not on the Medicare benefits schedule, meaning hospitals had to pay for the procedure out-of-pocket and cardiologists could only perform the incision on those who were “inoperable“.
“Patients are now able to have it regardless of surgical risk – and basically the patient population is patients over 70 who have varied comorbiditities or other past medical history,“ he said,
“It allows patient preference in terms of treatment to come into play, which prior to this was not feasible because of hospital constraints and the ability to do low-risk patients as per Medicare.“
With the new indication, Dr Adams said his hospital could expand its lists, heart team, and extend the option to more patients.
“When someone has a TAVI in our particular cohort, 72 per cent of our patients go home the next day, which is quite extraordinary, because it means that, especially [during the pandemic], we’re not putting pressure on the hospital system,“ he said.
He also predicted the costs of a TAVI, prior to this announcement, would be up to $50,000 in Melbourne if a patient was not deemed suitable for the procedure in a public hospital.
“We do around 100 a year at the moment and will do up to 200 in the next five to 10 years,“ he said.
“Improved access will also lead to benefits, not not just for us but also for research and development for getting better quality devices and better quality adjunct devices to reduce the risk of complication.“
Phil Holmes, who recently bought an acre of land in Glenda Ruel, about 25 minutes outside of Ballarat, said he has been given another 20 to 30 years of life and is enjoying the time he has left.
Of the estimated 66,500 Australians living with aortic stenosis, nine in 10 are not undergoing treatment each year, according to a recently published Ipsos survey.
“It’s so important that you listen to your body, and men in particular don’t like going to the doctor and talking about things – but they should, and it’s nothing to be ashamed of,“ Phil said.